3D Bioprinting: Shaping the Future of Organ Transplantation
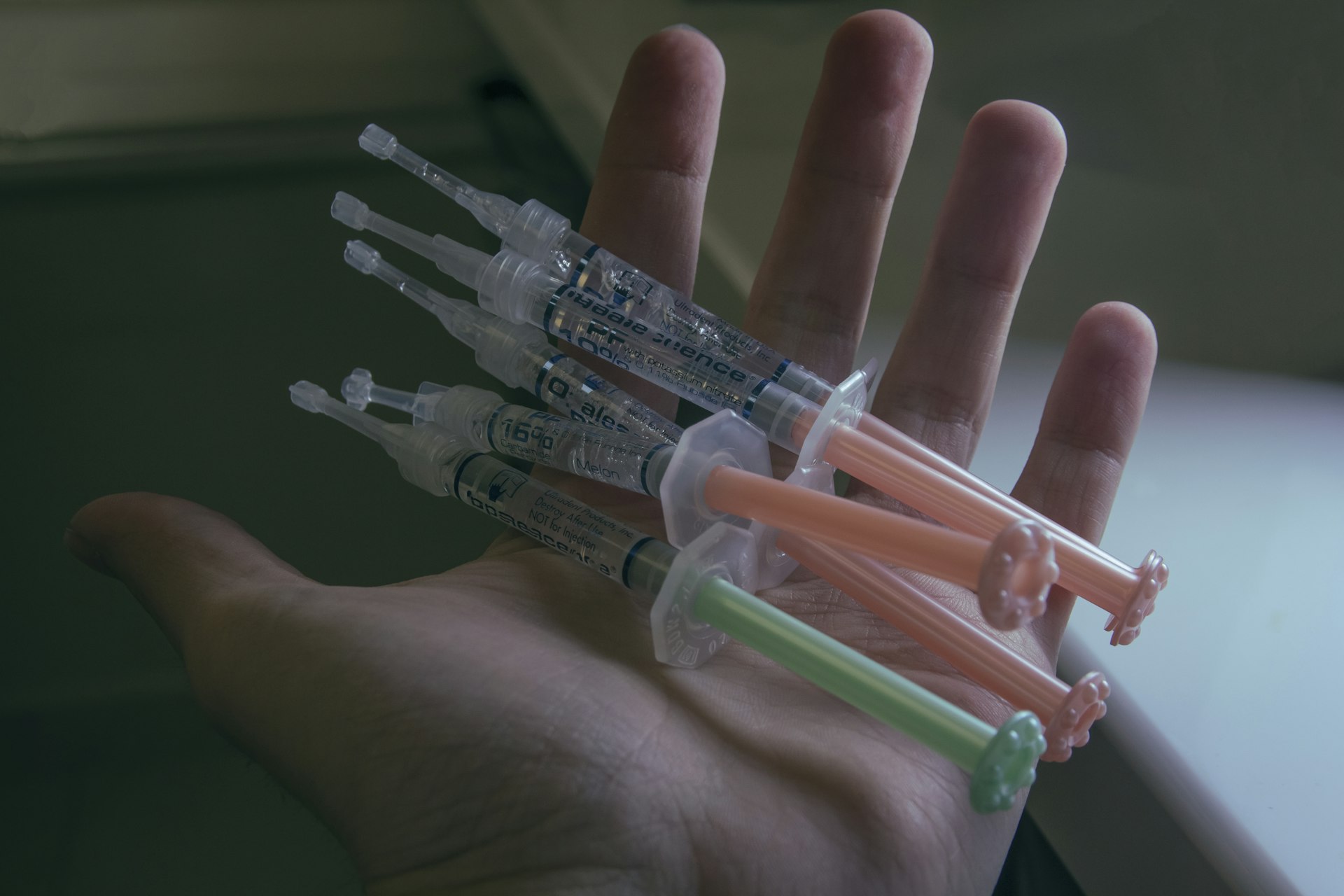

Photo by Ozkan Guner on Unsplash
Introduction: The Evolving Landscape of Organ Transplantation
Organ transplantation has long been the gold standard for treating end-stage organ failure, yet the persistent shortage of viable donor organs remains a life-threatening barrier for thousands worldwide. Traditional transplantation not only faces supply constraints but also carries risks of immune rejection, long waiting periods, and ethical dilemmas. In recent years, 3D bioprinting has emerged as a transformative technology poised to address these challenges and redefine the future of organ transplantation [1] .
Understanding 3D Bioprinting: Process and Promise
Unlike conventional 3D printing, which uses plastics or metals, 3D bioprinting employs bio-ink -a material composed of living cells and supportive hydrogels. The process begins with creating a digital blueprint of the organ, often derived from high-resolution imaging such as MRI or CT scans. This digital model guides the bioprinter, which deposits bio-ink layer by layer, building up the organ’s complex structure. After printing, the organ is placed in a bioreactor to promote cell growth and maturation, ensuring the tissue becomes functional and viable for transplantation [1] [2] .

Photo by CDC on Unsplash
Practical Implementation Steps
- Obtain high-resolution imaging of the patient’s organ (MRI/CT scan).
- Collaborate with bioengineers to create a precise digital model.
- Prepare bio-ink using the patient’s own cells, cultured and mixed with hydrogels.
- Utilize a specialized 3D bioprinter to fabricate the organ layer by layer.
- Place the printed organ in a bioreactor for maturation and functional validation.
Medical centers and research institutions with advanced tissue engineering departments are typically the first points of contact for accessing bioprinting services. You can inquire about eligibility for clinical trials or collaborative research by contacting these institutions directly or searching for “3D bioprinting clinical trials” through medical databases or university hospital websites.
Key Benefits of 3D Bioprinting in Transplantation
3D bioprinting offers several critical advantages:
- Unlimited organ supply: By printing organs on demand, the chronic shortage of donor organs could be mitigated, potentially saving countless lives [1] .
- Reduced rejection risk: Organs printed from the patient’s own cells minimize immune response and the need for lifelong immunosuppression, leading to better long-term outcomes [4] .
- Faster transplantation: Eliminating donor matching and waiting periods allows for timely interventions when patients need them most [1] .
- Ethical and legal improvements: With bioprinting, the black market for organs and ethical complexities of donor procurement could be significantly reduced [1] .
These benefits are not merely theoretical-real-world examples include successful transplantation of bioprinted bladders and windpipes, demonstrating the technology’s clinical viability [2] .
Recent Advancements and Case Studies
The field has witnessed several landmark achievements:
- In the early 2000s, a patient received a functional bladder bioprinted from his own cells.
- In 2022, a woman born without an ear received a 3D-printed ear implant fabricated with her own cartilage cells [2] .
- Bioprinted windpipe transplants have shown promise for patients recovering from thyroid cancer.
To learn more about ongoing clinical trials or technological updates, you can visit the websites of leading research hospitals or search for “clinical trials in 3D bioprinting” using databases like ClinicalTrials.gov.
Challenges and Limitations
Despite its promise, 3D bioprinting faces significant scientific, technical, and regulatory challenges:
- Complex organ architecture: Printing organs with intricate vascular networks and multiple cell types requires ongoing innovation in bioink composition and printing technology [5] .
- Functional validation: Each bioprinted organ must undergo rigorous testing to ensure it performs necessary biological functions, such as protein production in liver tissues [3] .
- Regulatory and ethical issues: The medical community is working to establish safety protocols, regulatory standards, and ethical guidelines for bioprinted organs. As with any new technology, approval processes can be lengthy, and access may be limited to research settings initially [5] .
Patients and practitioners interested in the latest guidelines should consult regulatory agencies such as the U.S. Food and Drug Administration (FDA) and search for updates on “bioprinting regulation” through their official portals.
Actionable Steps for Accessing 3D Bioprinting Technologies
Given the emerging nature of this field, here are practical pathways to engage with 3D bioprinting in organ transplantation:
- Contact major academic medical centers or research hospitals with regenerative medicine programs. Use search terms such as “regenerative medicine” or “tissue engineering” alongside your location to find relevant institutions.
- Look for clinical trial opportunities by searching “3D bioprinting organ transplant trials” on reputable databases like ClinicalTrials.gov.
- Engage with professional organizations such as the Organ Donation Alliance and the American Society of Transplantation for updates on technology integration and new initiatives.
- If you are a healthcare professional, consider professional development courses or workshops in tissue engineering and bioprinting offered by universities and biotech firms.
Individuals should be aware that access to bioprinted organs is still limited to research and early clinical settings. Eligibility typically involves meeting strict inclusion criteria and participating in carefully monitored studies.
Alternative Approaches and Future Directions
While 3D bioprinting holds immense promise, alternative approaches in transplantation are also being pursued, including xenotransplantation (using animal organs) and stem cell-derived organoids. Each method offers unique benefits and challenges, and ongoing research is essential to determine which solutions will be most effective and widely adopted [2] .
The future will likely see a combination of these technologies, with bioprinting leading the way toward personalized, on-demand organ replacement. Collaboration among scientists, clinicians, engineers, and policymakers is vital to overcome barriers and ensure safe, equitable deployment of these innovations [5] .
Key Takeaways and Next Steps
3D bioprinting is revolutionizing organ transplantation by offering solutions to donor shortages, reducing rejection risks, and paving the way for personalized medicine. While widespread clinical adoption is still on the horizon, patients and professionals can stay informed, participate in research, and connect with leading institutions to be part of this transformative shift.
For those seeking to access these technologies, the most effective strategy is to contact major research hospitals, search for clinical trials, and stay updated via professional organizations and regulatory bodies. As advancements continue, opportunities to benefit from bioprinted organs will expand, offering hope to millions facing organ failure worldwide.
References
- [1] Aumet (2025). Organ Transplantation From 3D Bioprinting.
- [2] Labiotech.eu (2024). The future of organ transplants: Xenotransplantation, 3D bioprinting, stem cells.
- [3] Organ Donation Alliance (2024). 3D Bioprinted Tissues for Organ Transplantation – Where Are We?
- [4] PMC (2020). 3D Bioprinting and the Future of Surgery.
- [5] RI Journals (2025). The Future of Organ Transplants: 3D Bioprinting and Beyond.






